
My friends and I often engage in organ recitals — Not the musical type but rather what is hurting today and can it be fixed. Doctoring is my new primary activity. I remember my late aunt telling me, after she moved into a retirement home, that when people ask how you are, they really don’t want an answer. Everybody hurts, so just say “fine” and move on.
My friends and I often engage in organ recitals — Not the musical type but rather what is hurting today and can it be fixed.
The new year brought me pain instead of a fresh start. Despite working with a physical therapist weekly, my old joints, beaten down by arthritis and a bad back, decided it was time for what my doctors call a “flare up.” On January 19-22, I was hospitalized for pain management due to sciatica, shoulder pain, and pseudo-gout (not a fake thing, but gout in my right knee caused by calcium crystals rather than the urate crystals of regular gout). After leaving the hospital, my pain doctor gave me another epidural injection in my back on January 23, which helped with the sciatica pain. It also hurt so much I almost jumped off of the table.
Since then, my focus has been on the knee pain, caused by the pseudo-gout. My rheumatologist drained fluid from and shot steroids into the knee on February 22 and again on March 19, April 8, and April 18. She also prescribed more pills.
Unfortunately, I have two sources of pain and can’t tell which one is the culprit. Recently, I had strong back pain in the morning, which subsided during the day after I took all of my meds. But the pain also radiated from the back of my right knee up my leg whenever I got up from sitting, making walking painful. My two doctors can duke it out over the next couple of weeks. All I want is for them to figure out who’s in charge and make me feel better.
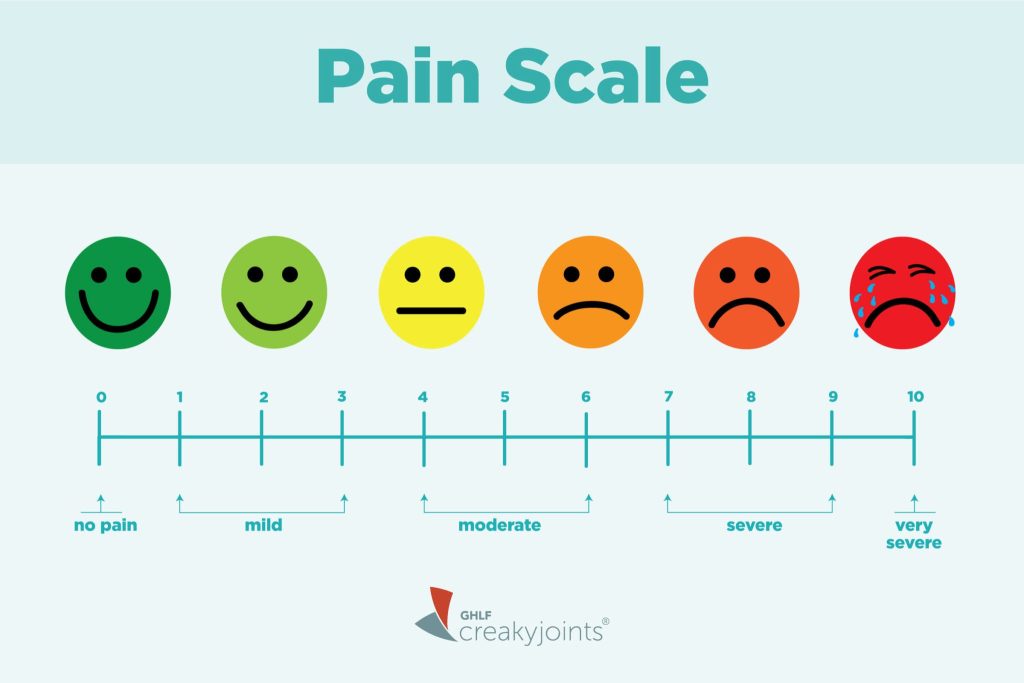
Despite efforts to make people’s perception of pain quantifiable or more objective (think all of those pain scale ratings, zero being no pain and 10 being the worst), how people experience and rate their pain is totally subjective. Some of us have higher thresholds for pain, while others are very sensitive to any discomfort. I don’t know where I fall on this spectrum, but I do know being asked to rate my pain is challenging and often useless.
For one thing, I know the numbers I give will affect Medicare’s coverage for procedures, especially for PT. So, I have to start with a relatively high number so I can show progress (or lack thereof) to justify my treatment. At one pain clinic where I was being treated for back pain, I was encouraged to rate myself high on the pain scale before receiving treatment and low after to indicate that the injection was successful. What no one ever told me there was that at one point they wanted me to fail to justify a more expensive procedure, so they did not give me anything more than lidocaine. Once I saw what the plan was, I found a new doctor.
A quote I particularly like, often attributed to Einstein but probably originating from William Bruce Cameron, tells us, “Not everything that counts can be counted, and not everything that can be counted counts.” I usually apply it to standardized testing, but I think the pain scale is also a reasonable application. I often ponder if 6 is good enough to be taken seriously. Should I say 7 or 8 or even 9 to get some treatment?
While I appreciate the need to measure pain to assess progress or lack of it in treating something that is hurting me, especially as I age, I find the need to quantify it bewildering. Also, if the answer I give relates to the medication I will receive for pain relief, I fear some of my doctors are too quick to prescribe opiates if the number I give is on the high side, while others will only suggest only Tylenol for a rating of 5.
All of this leaves me confused when asked, “How do you rate your pain?” Some time ago, I had a very sharp pain in my shoulder that rendered my left arm useless. For that one, I told my pain doctor’s scheduler I was a 9, which resulted in an appointment in a few days. But at my age, something always hurts, and living with a lower level of pain is the norm. The number I assign to my pain depends on the result I hope to achieve in seeing a doctor and receiving treatment.
Boomer. Educator. Advocate. Eclectic topics: grandkids, special needs, values, aging, loss, & whatever. Author: Terribly Strange and Wonderfully Real.


Ouch.
Oh Laurie, I feel your pain but only slightly! As I wrote this week , I’ve had a bout with sciatica, and was successfully treated – but by a very creepy doctor!
I hope you get some relief!
Thanks, Dana.
Excellent critique of the attempts to quantify pain, and oh so sorry to hear of your ongoing misery. Pain is indeed subjective, but real, and attempts to treat it depend on some consistency in reports—hence the scourge of the scales. There is no doubt that love and understanding are necessary components of any treatment. Sending you as much as I can.
Thanks, Khati. This year thus far has had its challenges, but I’m basically doing ok.
Wow, if anyone deserves to offer an organ recital!
As one who has questioned the use of “standardized data’ as a way of assessing learning, i am right behind you in the march to also de-legitimize this silly numerical approach to pain. I tolerate pain very well but does that mean I should never be offered meds? Ridiculous.
We all know that these numbers are arbitrary and doctors use them to justify medicare covering procedures.